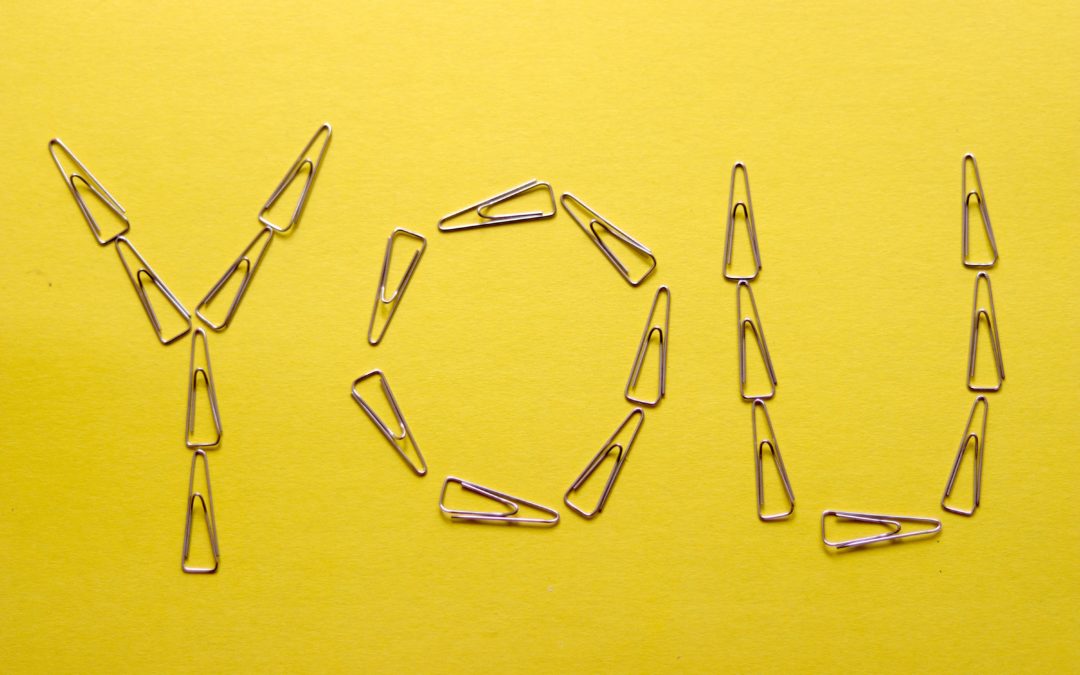
Four words that mean so much. Four words we use every day. Four words that can help us to get to
know each other. Four words that can break down barriers. Four words that we can shy away from.
Four words which we can be frightened of. Four words that can help to create that trusting therapeutic
relationship between nurse and patient. Four words that can open an abundance of questions. Four
words that can aid us to learn so much. Four words which help us to get to know what is important to
our patients. Four words which can be overlooked. Four words in which we need to listen to the answer.
Four words to me which are the heart of holistic assessment and person-centred care.
Modern nursing and medicine’s true healing potential depends on a resource that is being
systematically depleted: the time to truly listen to patients, hear their stories, and learn not only what’s
the matter with them but also what matters to them. However, some health professionals, including
nurses, claim that workload and staffing shortages have compressed encounters to a point that genuine
conversation with patients is no longer possible. Compressed nursing has real risks. Clinicians become
more likely to provide ineffective treatment and miss pertinent information that would have altered the
treatment plan and can often be blind to patients’ lack of understanding. All of this serves to diminish
the joy of serving patients, thereby contributing to high rates of staff burnout. These consequences have
clear human costs.
We are more likely to respond honestly to ‘Tell me about you?’ within our own comfort zones -our
homes. Therefore, community-based neighbourhood teams, including District Nurses, are professionals
who are most likely to have the most honest and open conversations with patients, families and carers.
The District Nursing Service provides nursing care and support for patients, families and carers in
homes and communities in every part of the UK (The Queens Nursing Institute, 2016). District Nursing
services often act like a ‘sponge’, absorbing additional workload in an environment without the physical
limits of a defined number of beds and, in my opinion, are the true heroes and advocates for patients
within our communities.
District nursing services provide a lifeline for many people and play a key role in helping them to
maintain their independence, manage long-term conditions and treat acute illnesses. At their best, they
deliver an ideal model of person-centred, preventative and co-ordinated care, which can reduce hospital
admissions and enable people to stay in their own homes. While demand for services has been
increasing, available data on the workforce indicates that the number of nurses working in community
health services has declined over recent years, and the number working in senior ‘District Nurse’ posts
has fallen dramatically over a sustained period (Maybin et al, 2016). Vital investment is required to help
retain our District Nurse workforce, build much more capacity in the system to allow them to spend
more time with our patients and to provide them with a professional career development pathway.
Buurtzorg Britain and Ireland are currently helping purpose driven organisations produce great
outcomes in sustainable ways through self-managed teams. To date, they have supported change in
more than 30 organisations in Britain and Ireland, spanning the NHS, local government, social
enterprises and charities. Buurtzorg, a model of community nursing conceived in the Netherlands, is
widely cited as a promising and evidence-based approach to improving the delivery of integrated
nursing and social care in community settings. The model is characterised by high levels of patient and
staff satisfaction, professional autonomy exercised through self-managing nursing teams, client
empowerment and holistic, patient centred care (Lalani, 2019). Whilst many of the principles of the
Buurtzorg model are applicable and transferable to the UK, in particular promoting independence
among patients, improving patient experience and empowering frontline staff, the successful
embedding of these aims as normalised ways of working will require a significant cultural shift at all
levels of the NHS.
The ‘First Coffee then Care’ mantra of Buurtzorg is one which for me can allow their neighbourhood
teams to really dedicate themselves to the ‘Tell me about you?’ paradigm. This approach helps the
nurse to get to know the patient and appreciate their history with a personal and individualised
approach. Whilst the multi-tasking skill of healthcare professionals in our healthcare settings today is to
be applauded, ‘can you truly listen to anyone and do anything else at the same time?’ (Peck, 1978).
The ‘Tell me about you?’ question requires time to listen to the answer. Time – something that we seem
to have less and less of in today’s modern world. If you have the time or can make the time, please ask
the question, ‘Tell me about you?’. Four words. Four words that mean so much.
Liam Redden 
Lecturer/Senior Lecturer School of Health and Life Sciences, Teesside University
MSc Specialist Practice in District Nursing
Registered Nurse (Adult)
References:
Lalani, M., Fernandes, J., Fradgley, R., Ogunsola, C. Marshall, M. (2019). Transforming community nursing services in the UK: lessons from a participatory evaluation of the implementation of a new model of community nursing in East London, BMC Health Services Research, 19, pp.945.
Maybin, J., Charles, A., Honeyman, M. (2016). Understanding quality in district nursing services.Learning from patients, carers and staff. London, The Kings Fund.
Peck. M.S. (1978). The Road Less Traveled: A New Psychology of Love, Traditional Values, and
Spiritual Growth. New York, Simon & Schuster.
The Queens Nursing Institute. (2016). Understanding safe caseloads in the District Nursing service A
Q).NI Report. London, The Queens Nursing Institute.